KEY TAKEAWAYS
- The study aimed to investigate the enhanced efficacy of TIL therapy by utilizing agonistic anti-4-1BB and CD3 antibodies in early ex vivo TIL culture.
- The primary endpoint was to evaluate the ORR.
- Researchers noticed the feasibility of TIL manufacturing with 4-1BB and CD3 agonism, demonstrating safety and early immunological effects; further research is required.
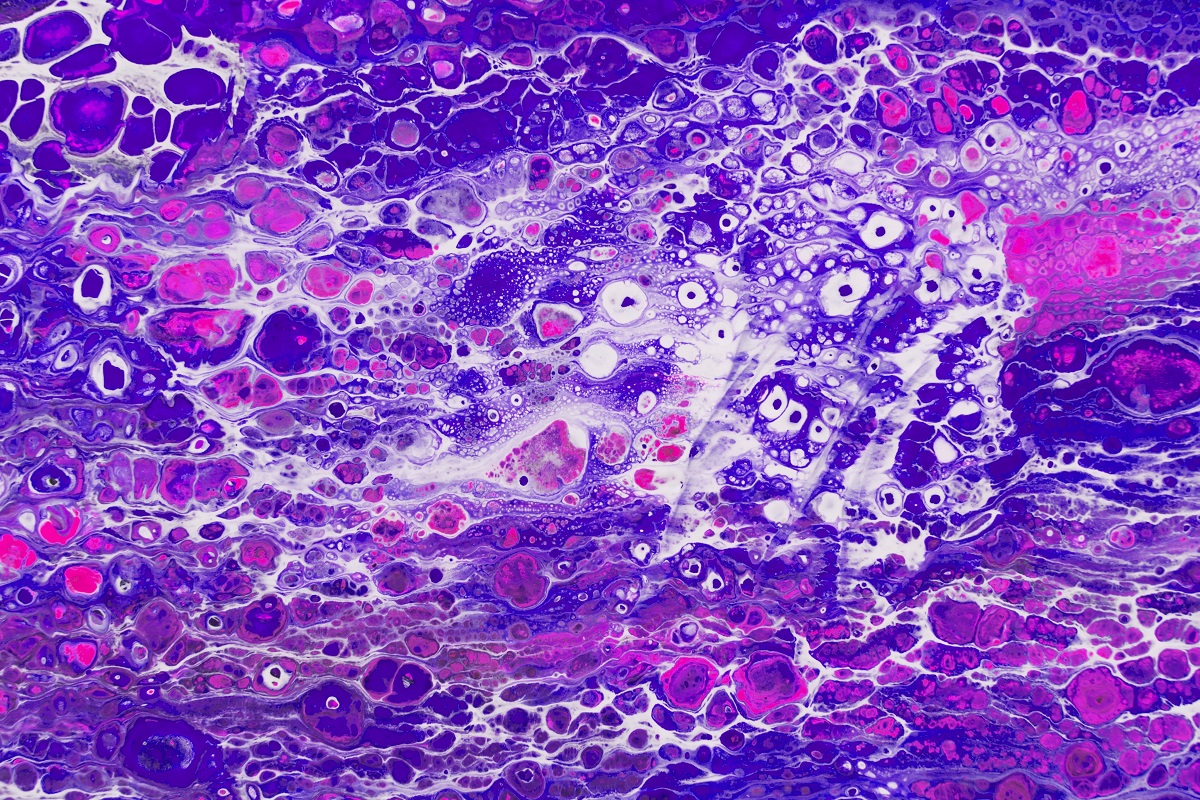
Tumor-infiltrating lymphocyte (TIL) therapy has emerged as a promising treatment modality for metastatic melanoma, non-small cell lung cancer, and various solid tumors. Rodabe Amaria and her team’s prior preclinical investigations revealed that the early ex vivo TIL culture, assisted by agonistic anti-4-1BB and CD3 antibodies, led to a more robust production of CD8-predominant TILs.
They performed an inclusive analysis encompassing patients (pts) with treatment-refractory metastatic colorectal (CRC), pancreatic (PDAC), and ovarian (OVCA) cancers. Eligible pts underwent lymphodepleting chemotherapy followed by ex vivo expanded TIL infusion, manufactured at MD Anderson Cancer Center with IL-2 and agonistic stimulation of CD3 and 4-1BB (urelumab). Subsequently, pts received up to six doses of high-dose IL-2 following TIL infusion. The primary endpoint was evaluating the objective response rate at 12 weeks, utilizing Response Evaluation Criteria in Solid Tumors version 1.1. Secondary endpoints included disease control rate (DCR), duration of response, progression-free survival (PFS), overall survival (OS), and safety.
About 17 pts underwent TIL harvest, and 16 were treated on the protocol, comprising 8 CRC, 5 PDAC, and 3 OVCA pts. The median age was 57.5 (range 33-70), with 50% females. Median prior therapy lines were 2 (range 1-8). No responses were observed at 12 weeks, but 10 subjects achieved at least one stable disease (SD) assessment, resulting in a DCR of 62.5% (95% CI 35.4% to 84.8%). The best response included prolonged SD in a PDAC patient lasting 17 months. Median PFS and OS across cohorts were 2.53 months (95% CI 1.54 to 4.11) and 18.86 months (95% CI 4.86 to NR), respectively. Grade 3 or higher toxicities attributable to therapy were seen in 14 subjects (87.5%; 95% CI 61.7% to 98.4%). Infusion product analysis revealed the presence of effector memory cells with high CD39 expression, irrespective of tumor type, and low expression of checkpoint markers.
The study concluded that TIL manufacturing with assistance from 4-1BB and CD3 agonism is feasible and demonstrated no new safety signals. Despite the absence of observable responses, a notable proportion of pts achieved SD, indicating an early or partial immunological effect. Further research is required to identify resistance factors and enhance T cell functionality, paving the way for a more effective therapy.
Source: https://pubmed.ncbi.nlm.nih.gov/38309721/
Amaria R, Knisely A, Vining D, et al (2024). Efficacy and safety of autologous tumor-infiltrating lymphocytes in recurrent or refractory ovarian cancer, colorectal cancer, and pancreatic ductal adenocarcinoma. J Immunother Cancer. 2024 Feb 2;12(2):e006822. doi: 10.1136/jitc-2023-006822. PMID: 38309721; PMCID: PMC10840042.