KEY TAKEAWAYS
- The PUBMIC interventional trial aimed to evaluate the impact of sarcopenia and body fat metrics on radiologic parastomal hernia incidence post-cystectomy.
- The results demonstrated that the increased subcutaneous fat raises the risk of post-surgical fluid collection in bladder cancer patients, while other potential factors do not appear influential.
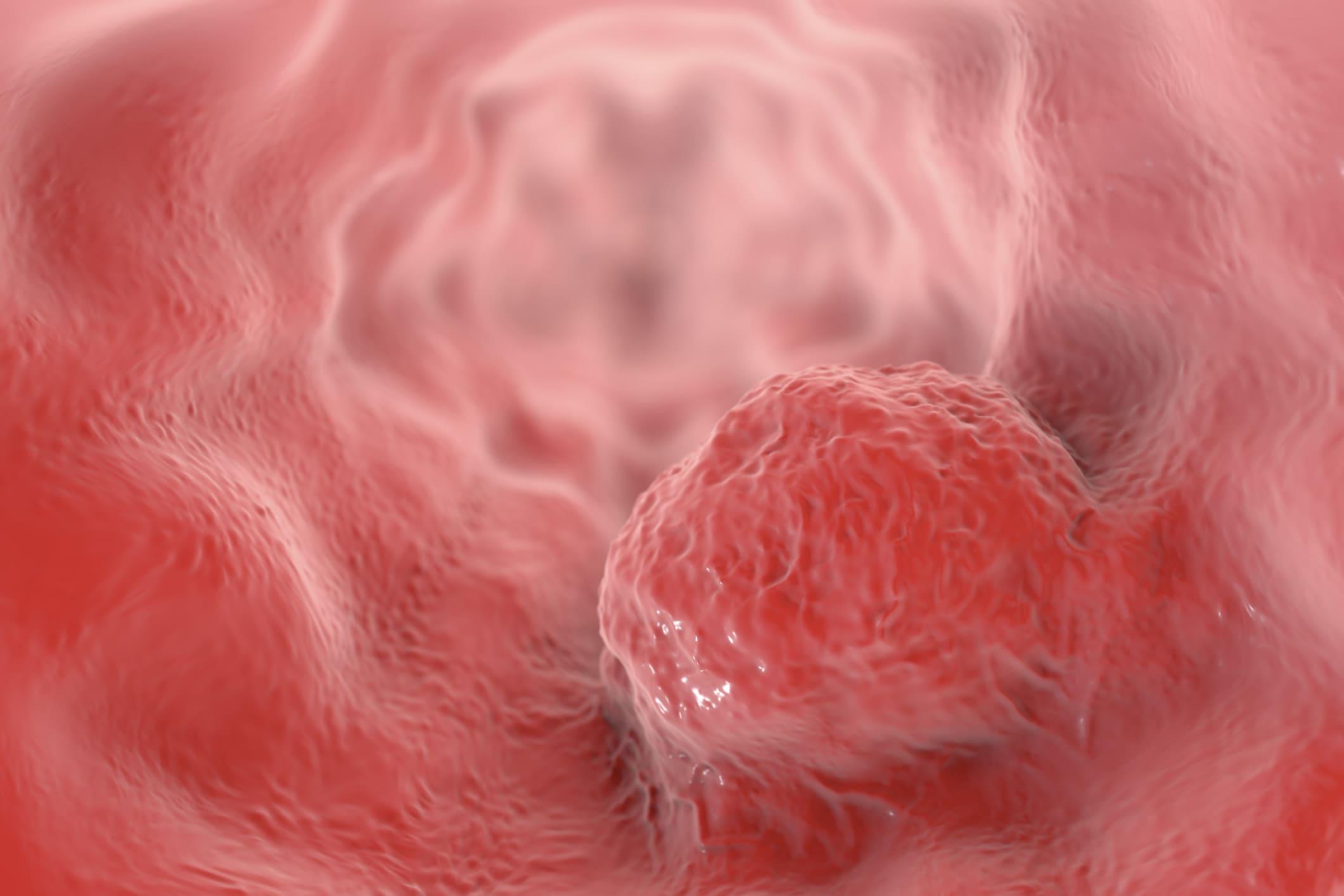
Cystectomy patients often rely on ileal conduits (IC) for urinary diversion, but this procedure carries a high risk of a debilitating complication: parastomal hernia (PSH). While known risk factors exist, the influence of musculoskeletal health on PSH remains uncertain. Limited data hinders understanding how muscle strength, bone density, or other skeletal metrics might contribute to PSH development.
Alireza Ghoreifi and his research team spearheaded the study that aimed to investigate the potential role of sarcopenia and body fat metrics as predictors for radiologic PSH following cystectomy, aiming to improve patient selection and surgical planning.
The study retrospectively analyzed clinical data and preoperative abdominopelvic CT scans from participants in the Prophylactic Use of Biologic Mesh in Ileal Conduit (PUBMIC) trial (NCT02439060). Exclusions included scans older than 3 months and cases with severe body deformities hindering musculoskeletal metric calculations. Utilizing Synapse 3D software, under the guidance of a blinded experienced radiologist, they calculated visceral fat area (VFA), subcutaneous fat area (SFA), and waist circumference (WC) at upper-L3 and umbilicus levels. Psoas muscle area (PMA) at L3 determined sarcopenia (lowest sex-specific quartile of psoas muscle index, PMI: PMA/Ht2). Cox regression analysis assessed associations between muscle/fat metrics and radiologic PSH risk.
Among 137 eligible patients from the PUBMIC trial, with a median age of 75 (IQR: 71-80) years and 74% being male, 25% developed radiologic PSH during a median follow-up of 22 months. Preoperative sarcopenia, defined by PMI cutoffs, showed no association with PSH development (HR 0.6, 95% CI 0.3-1.5, P=0.3). Univariate analysis revealed prior abdominal radiation as the only clinical variable associated with PSH (HR 3.2, 95% CI 1.1-9.1; P=0.03). In multivariable analysis, SFA at L3 > 220 cm2 (Q3) significantly increased the risk of PSH (HR: 2.5, 95% CI 1.2-5.2; P=0.01).
The results showed that cystectomy patients with greater pre-operative subcutaneous fat area were significantly more likely to develop radiologic PSH than those with less, emphasizing the significant link between this fat metric and PSH risk. The study was sponsored by the University of Southern California.
Source: https://suo-abstracts.secure-platform.com/a/gallery/rounds/18/details/3197
Clinical Trial: https://clinicaltrials.gov/study/NCT02439060
Ghoreifi A, Kumar SS, Le J, et al.’’ SUBCUTANEOUS FAT AREA AS A RISK FACTOR FOR PARASTOMAL HERNIA FOLLOWING CYSTECTOMY AND ILEAL CONDUIT: DATA FROM THE PUBMIC TRIAL.’’ Presented at: SUO 2023 (Poster #76)