KEY TAKEAWAYS
- The study aimed to assess macrophage-based immunotherapy’s impact on survival in patients with unmethylated MGMT glioblastoma.
- Researchers noticed Temferon’s promising safety profile and its potential to mitigate disease progression in unmethylated MGMT glioblastoma, offering hope for improved therapeutic outcomes.
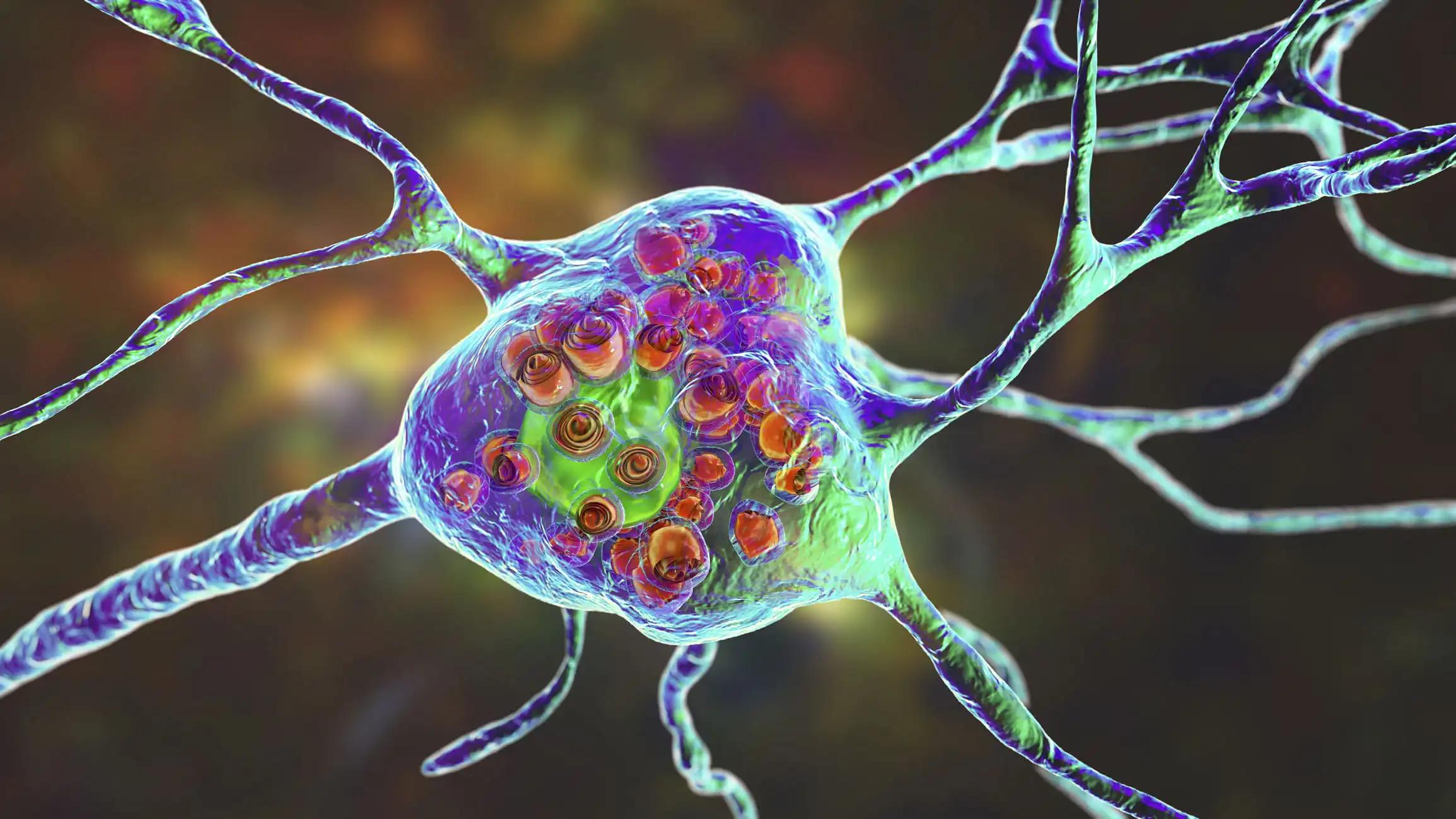
Glioblastoma multiforme (GBM) is a form of brain cancer that is an incurable glial tumor that affects the central nervous system. Patients with unmethylated MGMT promoter, a subgroup with a particularly unfavorable prognosis, exhibit a reported median survival of 12.7 months, with less than 15% surviving beyond 2 years. Despite the success of immunotherapies in slowing or eradicating various tumors, including those metastasized to the brain, GBM remains a formidable challenge, with no significant survival extension achieved thus far.
Francesca Farina and the team aimed to assess the potential of a novel macrophage-based immunotherapy, Temferon, in improving survival outcomes for patients with unmethylated MGMT GBM.
Researchers performed an inclusive analysis, conducting a Phase 1/2a dose-escalating non-randomized open-label study in newly diagnosed GBM multiforme with unmethylated MGMT gene promoter. This study involved an i.v. injection of autologous CD34+ HSPCs genetically modified with a lentiviral vector encoding for human interferon-a2 (Temferon). Temferon was designed to deliver IFN-α2 within the TME by Tie-2 expressing macrophages (TEMs).
The study aimed to evaluate the short-term (up to 90 days) and long-term (up to 2 years) tolerability and safety of five escalating doses of Temferon in up to 27 GBM patients. Autologous CD34+ HSPCs were mobilized with lenograstim and plerixafor, collected by apheresis, purified, and ex vivo modified with a lentiviral vector.
Following a sub-myeloablative conditioning regimen (Thiotepa + BCNU or Thiotepa + Busulfan or Busulfan alone), up to 3 million Temferon cells/kg were administered following a fixed dose of non-manipulated CD34+ supporter cells.
About the results, as of 27 July 2023, 21 GBM patients in 7 cohorts received incremental doses of Temferon up to 3 million cells/kg, and 5 patients were still alive with a median OS of 17 months and a median PFS of 8.3 months following initial surgery. To date, no DLTs have been identified. In all patients, rapid engraftment of modified progenitors and fast hematological recovery were observed within two weeks of transplantation.
Grade 4 or 5 serious adverse events (n=7 patients), including graft failure, febrile neutropenia, pneumonia, steroid restart, and disease progression, were mostly attributed to the conditioning chemotherapy, but steroid usage or disease progression was also listed. 1 SUSAR (persistent GGT elevation) occurred.
The higher transduced cell proportion in the BM was observed 30 days after Temefron administration, with a chimerism for the highest dose tested at up to 40%, still detectable in the long-term. Very low concentrations of IFNa were detected in the plasma, indicating a tight regulation of vector expression. Seven patients underwent second surgery, and genetically engineered cells (6 out of 7 patients assessed) were detected within the bulk tumor lesion (>3% in 3 patients). Moreover, IFN-responsive genes were up-regulated, suggesting a local IFNα release by TEMs.
In 1 patient, a stable lesion had a higher proportion of T cells & TEMs, an increased IFN-response signature, and myeloid re-programming revealed by scRNAseq compared to a synchronous, progressing tumor. TCR sequencing of blood and tumor samples showed a post-treatment increase of peripherally expanded clone frequency in the tumor samples, as evidence of a crosstalk between peripheral and tumor repertoires of T cells.
The study concluded that the data support the initial evidence regarding the safety and tolerability of Temferon. Additionally, it suggests that Temferon holds promise in mitigating disease progression in patients afflicted by unmethylated MGMT GBM.
The study was sponsored by Genenta Science.
Source: https://ebmt2024.abstractserver.com/program/#/details/presentations/840
Clinical Trial: https://clinicaltrials.gov/study/NCT03866109
Farina F, Gentner B, Finocchiaro G, et al. (2024). “A MACROPHAGES-BASED IMMUNOTHERAPY OF SOLID TUMORS MICROENVIRONMENT: PRELIMINARY RESULTS OF THE TEM-GBM_01 STUDY.” Presented at EBMT 2024 (Abstract OS16-06).