KEY TAKEAWAYS
- The phase 2 trial aimed to investigate the efficacy and safety of ibrutinib combined with nivolumab for treating refractory CNS lymphoma.
- The primary endpoint was to determine ORR
- Researchers noticed significant clinical activity with ibrutinib and nivolumab in CNS lymphoma; further information will be provided later.
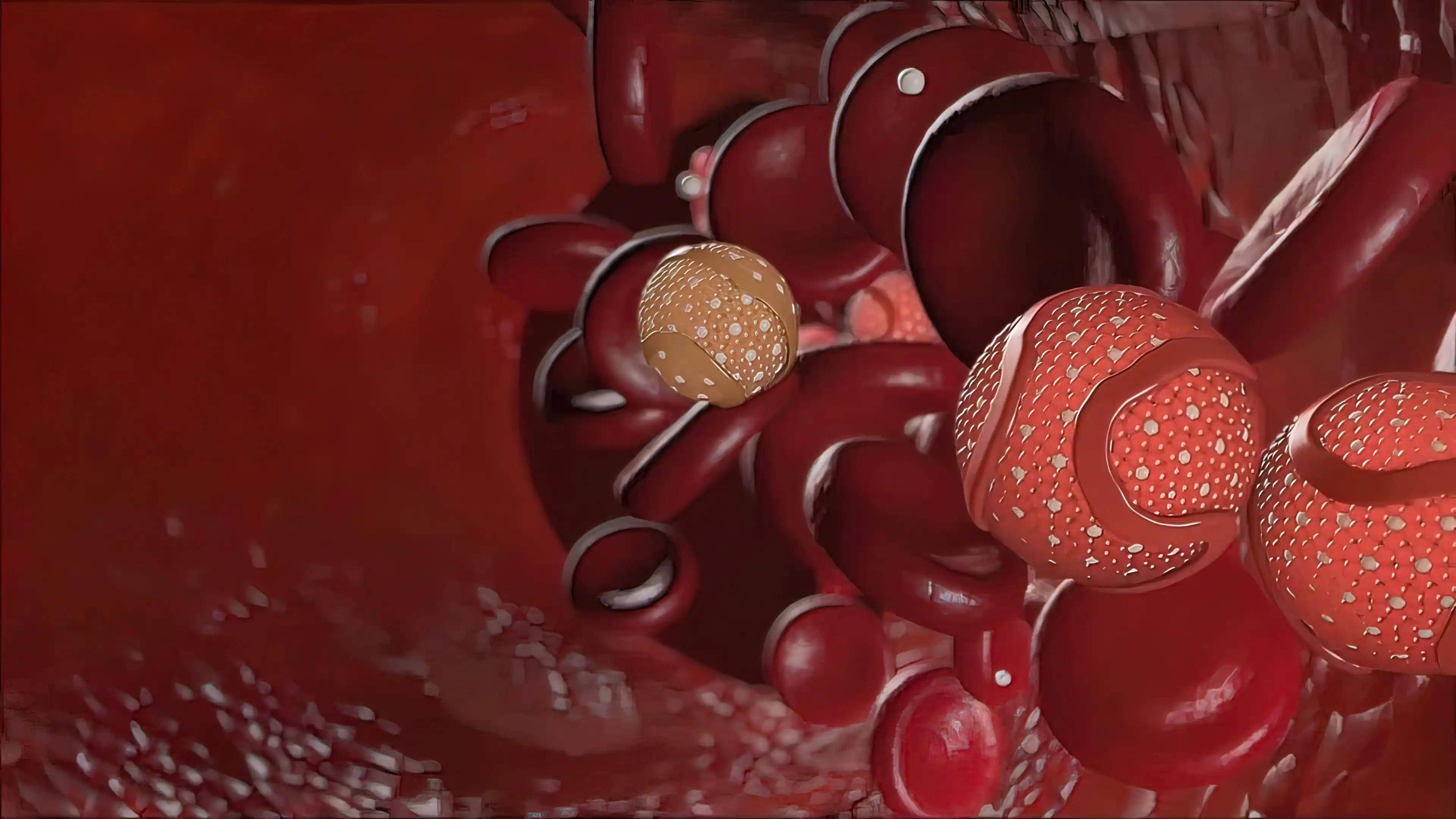
Central Nervous System (CNS) lymphoma, a distinct entity of large B-cell lymphoma (LBCL), exhibits a unique genomic profile akin to the activated B-cell (ABC) subtype, presenting potential therapeutic targets. Common aberrations, including MYD88 mutations and 9p24 alterations, suggest susceptibility to Bruton’s tyrosine kinase (BTK) inhibitors and PD-targeted therapies. Ibrutinib combined with nivolumab demonstrated safety and clinical efficacy in relapsed non-Hodgkin lymphoma/chronic lymphocytic leukemia, prompting investigation for CNS lymphoma.
Jason Westin and his team aimed to assess the potential of the ibrutinib combination with nivolumab, given the genomic similarities and therapeutic sensitivities identified.
The study performed an inclusive analysis through an investigator-initiated, open-label, single-center, phase 2 clinical trial (NCT03770416). Eligible adult patients (pts) with relapsed CNS lymphoma refractory to or relapsed after at least one prior CNS-directed therapy were enrolled. Criteria included adequate organ and bone marrow function, absence of prior ibrutinib or PD1 inhibitor therapy, and no requirement for persistent high-dose steroids. The trial comprised two sequentially enrolled cohorts: Cohort A initiated with ibrutinib 560 mg oral daily for one cycle, followed by ibrutinib combined with nivolumab 240 mg IV every 14 days.
Cohort B involved simultaneous administration of ibrutinib and nivolumab during the first cycle. Pts achieving a partial response or greater after 6 cycles could continue therapy for up to 2 years or until disease progression or unacceptable toxicity. The primary objective aimed to determine the best overall response rate (ORR) of ibrutinib and nivolumab. Secondary objectives included the ORR of ibrutinib as a lead-in, best complete response (CR) rate, landmark survival outcomes, and safety of the combination. Initially planning to enroll 20 pts in both cohorts A and B, the trial closed prematurely due to slow accrual, partly attributed to the COVID-19 pandemic.
About 18 pts with relapsed CNS lymphoma were accrued from February 2019 to June 2022, and all pts were evaluable for response. The median age was 63 years (range 43-88), with 33% aged >70 years, and 78% were female. Primary CNS lymphoma was seen in 89% of cases, with 50% having non-GCB, 22% GCB, and 28% unable to be classified due to missing components of the Hans algorithm. The median number of prior lines of therapy was 2 (range, 1-4), 55% had refractory disease, 17% had a prior stem cell transplant, and 11% had prior CAR T-cell therapy.
10 pts were enrolled in Cohort A (ibrutinib lead-in), and eight pts in Cohort B (initial combination therapy). Adverse events included fatigue (50%), nausea (33%), and mucositis (28%).
For both cohorts combined, the best ORR was 77.8% (95% CI: 52~94%) with a best CR rate of 50% (95% CI: 26-74%). In Cohort A, the ORR of ibrutinib as a lead-in after 1 cycle was 90% (95% CI: 55.5-99.7%), and the CR rate was 60%. Among GCB pts (n = 4), the ORR and CR rates were 25%, while in non-GCB pts (n = 9), the ORR and CR rates were 100% and 56%, respectively.
With a median follow-up time of 34.6 months, the median overall survival (OS) was 25.4 months (95% CI 12.5-NR), and the OS rate at 12 months was 70%.
The median progression-free survival (PFS) was 6.6 months (95% CI: 2.9 – NR), and the PFS rate at 18 months was 47%. 4 pts withdrew from protocol therapy in CR, including 2 who proceeded to stem cell transplant consolidation, and 2 who stopped due to fatigue. 3 pts withdrew from protocol therapy in PR, 2 due to mucositis, and one due to arthralgias. Unfortunately, 1 patient died of COVID-19 infection after achieving a complete response following 4 cycles of therapy.
The study concluded that ibrutinib and nivolumab resulted in significant clinical activity in pts grappling with refractory or relapsed CNS lymphoma. Despite the constraint of small patient numbers, the findings underscore the promise of targeted therapy combinations, pointing towards the need for exploration in more extensive clinical studies. Additional evaluation is ongoing.
The study is sponsored by M.D. Anderson Cancer Center
Source: https://ash.confex.com/ash/2023/webprogram/Paper191123.html
Clinical Trial: https://clinicaltrials.gov/study/NCT03770416
Westin J, Nair R, Fayad L, et al. (2023). “Nivolumab and Ibrutinib for Treatment of Patients with Refractory or Relapsed Central Nervous System Lymphoma.” Presented at ASH 2023 (Abstract 1721).