KEY TAKEAWAYS
- The phase II trial aimed to determine whether propranolol improves response to therapies in esophageal cancer pts.
- The primary endpoint was to determine the ORR. Secondary endpoints were safety, PFS, OS, and ORR.
- The study will enroll 37 pts to assess efficacy and biomarkers. The trial is currently open to enrollment.
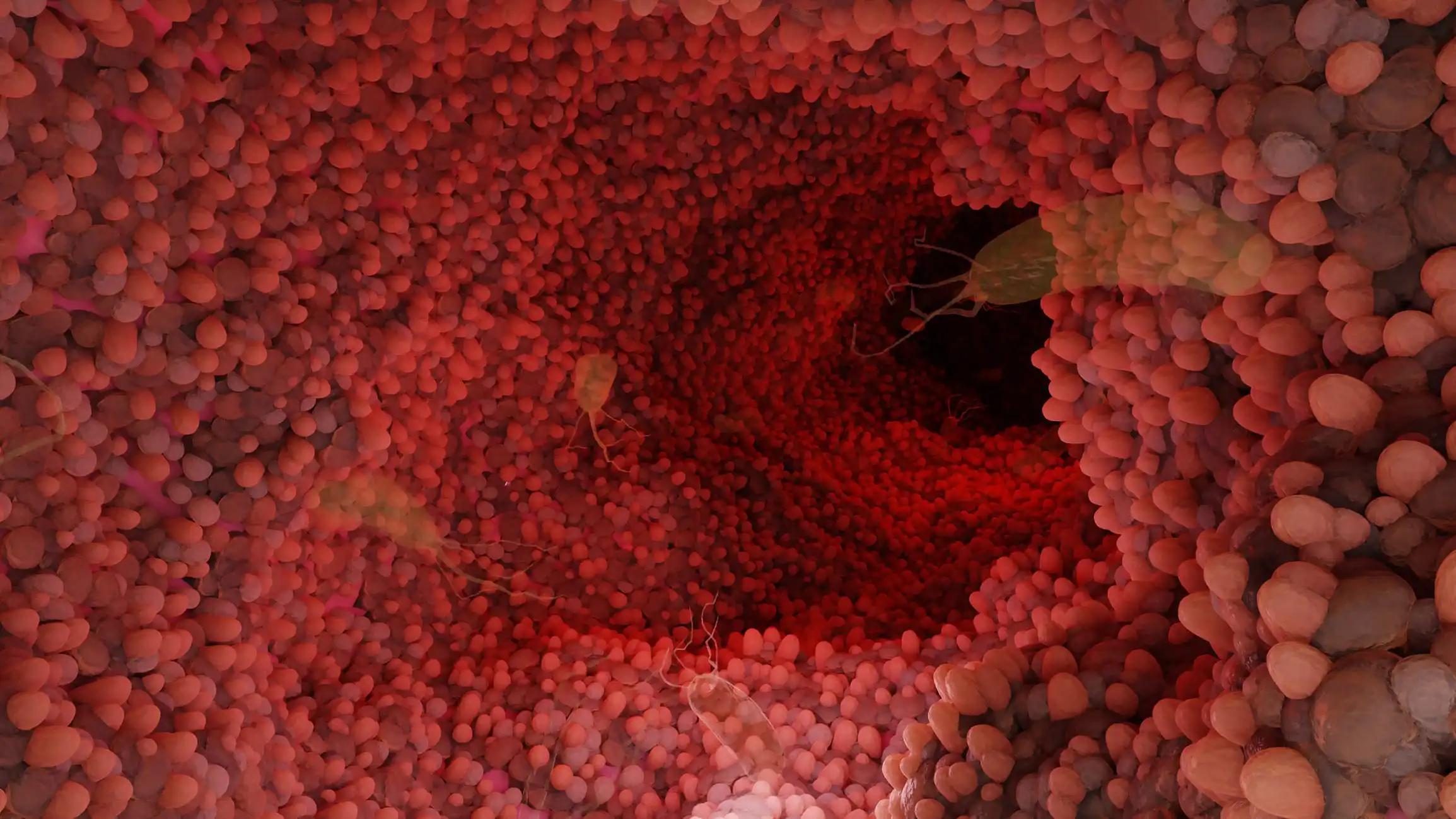
Chronic stress suppresses the immune system and promotes cancer growth. β-blockers (BB) may improve the efficacy of immune checkpoint inhibitors in animal studies and esophageal cancer patients(pts).
Researchers aimed to determine whether propranolol, a β-blocker, improves response to therapies in esophageal cancer pts.
The study included unresectable/metastatic esophageal/gastroesophageal junction adenocarcinoma(EGAC), treatment-naïve pts with good organ function and ECOG performance status of 0-1 who can participate if they take oral medication. Those with Her-2 positive cancer, active autoimmune diseases, HIV, Hepatitis B/C, or prior pneumonitis/interstitial lung disease requiring treatment are ineligible. Pts on β-blockers are also excluded. Eligible pts will receive mFOLFOX6 every 2 weeks alongside intravenous pembrolizumab (400 mg every six weeks) and oral propranolol (30 mg twice daily). mFOLFOX6 includes dl-LV, oxaliplatin, bolus 5-FU, and a 48-hour 5-FU infusion. The study will begin with a safety lead-in cohort of 6 pts.
The primary endpoint is the overall response rate (ORR) determined by RECIST 1.1. Secondary endpoints include safety, progression-free survival (PFS), overall survival (OS), and ORR as determined by iRECIST. Correlative studies will assess baseline levels or changes in the levels of biomarkers, such as peripheral T-cell subsets, myeloid-derived suppressor cells (MDSC), cytokines, and their association with efficacy endpoints (ORR, PFS, OS). The perceived stress scale (PSS) and the chronotropic effects of exercise will be examined for their potential impact on these efficacy measures.
The study requires 37 pts for evaluation, with the goal of achieving a 20% increase in the ORR compared to the historical ORR of 50% with standard treatment. In the first stage, 23 pts will be enrolled, and if 13 or more show a positive response, an additional 14 pts will be enrolled in the second stage. If 24 or more pts out of the 37 show a positive response, the new treatment will be considered promising for further research. The study is currently accepting patient enrollment.
Source: https://ascopubs.org/doi/abs/10.1200/JCO.2023.41.16_suppl.TPS4171?af=R
Clinical Trial: https://www.clinicaltrials.gov/study/NCT05651594
Sarbajit Mukherjee, Karan Jatwani, Sarah Chatley, Christos Fountzilas, Sylvia Vania Alarcon Velasco, Deepak Vadehra, Renuka V. Iyer, Kristopher Attwood, Mark Farrugia, Anurag K. Singh, and Elizabeth A. Repasky. DOI: 10.1200/JCO.2023.41.16_suppl.TPS4171 Journal of Clinical Oncology 41, no. 16_suppl (June 01, 2023) TPS4171-TPS4171.